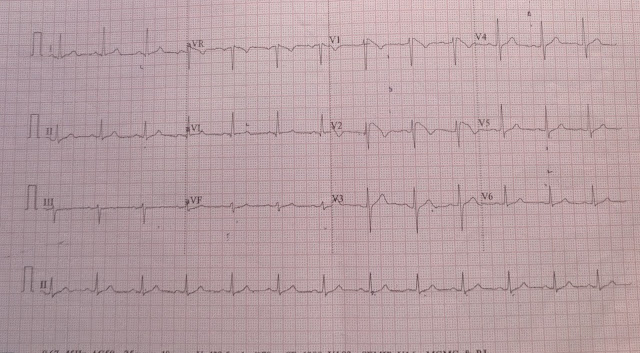
A 51-year-male came to JIPMER Pondicherry, India with chief complaints of giddiness since last one week. There were no history of syncope, palpitation, chest pain. There was no past history of diabetes mellitus, hypertension. ECG of the patient is shown below
Patient underwent EPS study and found to have complete heart block with atrial flutter arising from right atrium. Patient underwent successful radiofrequency ablation. In view of his Complete heart block he latter underwent successful permanent pacemaker implantation.
Thank you.
Typical atrial flutter (AFL) is a macroreentrant atrial tachycardia (AT) that uses the cavotricuspid isthmus as an essential part of its circuit. The circuit boundaries are the tricuspid annulus, crista terminalis, IVC, eustachian ridge, CS os, and probably the fossa ovalis. These barriers (lines of
conduction block) can be functional or anatomical, and are necessary to provide adequate path length for the flutter reentry circuit. The tricuspid annulus forms the anterior border of the flutter circuit,
whereas the posterior border occurs at a variable distance from this anterior border; it is narrowest in the region of the eustachian ridge and widest in the anterior part of the RA. Typical AFL is of two types, counterclockwise and clockwise.2 In counterclockwise AFL, activation proceeds caudocephalic up the septal side of the tricuspid annulus toward the crista terminalis and moves cephalocaudal along the lateral wall of the RA to reach the lateral tricuspid annulus, after which it propagates through the isthmus defined by the IVC, CS, and tricuspid annulus (counterclockwise as viewed in the left anterior oblique [LAO] view from the ventricular side of the tricuspid annulus). The circuit is entirely in the RA. In clockwise (reverse typical) AFL, activation propagates
in the opposite direction
ELECTROCARDIOGRAPHIC FEATURES
Typical Atrial Flutter P Waves. Flutter waves appear as atrial complexes of constant morphology, polarity, and CL. Typically, flutter waves are most prominent in the inferior leads (II, III, aVF)
and V1. In the inferior leads, they appear as a picket fence varieties coexist with tall positive, small positive, or biphasic (sawtooth) because the leads are primarily negative. This consists of a downsloping segment, followed by a sharper negative deflection, and then a sharp positive deflection,
with a positive overshoot leading to the next downsloping plateau. The relative size of each component can vary markedly. Counterclockwise AFL can be characterized by pure negative deflections in the inferior leads, negative and then positive deflections that are equal in size, or a small negative and then a larger positive deflection. Those three P waves in V1, respectively. The degree of positivity in the inferior leads appears to be related to the coexistence of heart disease and LA enlargement. Counterclockwise AFL will always have a negative deflection preceding the positive deflection in the inferior leads. Leads I and aVL characteristically show low-voltage deflections. Clockwise AFL generally has broad positive deflections in the inferior leads and wide negative deflections in V1.
Reference
Issa Z, Miller JM, Zipes DP. Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald's Heart Disease: Expert Consult: Online and Print. Elsevier Health Sciences; 2012 Apr 24.
ECG 1(Click on the image to enlarge it)
ECG is suggestive of heart rate of 38 beats per minute, atrial rate around 300 beats per minute, saw tooth P wave seen in lead V1, there is no definite baseline seen between P wave, P wave with saw tooth were negative in lead 2,3,avf suggestive of atrial flutter. The heart rate is nearly regular, no variability seen so the possibility in this patient is either Atrial flutter with block (6:1) (Counterclockwise typical flutter) or an underlying complete heart block.
Another ECG of the same patient (ECG 2)
Patient underwent EPS study and found to have complete heart block with atrial flutter arising from right atrium. Patient underwent successful radiofrequency ablation. In view of his Complete heart block he latter underwent successful permanent pacemaker implantation.
Thank you.
Typical atrial flutter (AFL) is a macroreentrant atrial tachycardia (AT) that uses the cavotricuspid isthmus as an essential part of its circuit. The circuit boundaries are the tricuspid annulus, crista terminalis, IVC, eustachian ridge, CS os, and probably the fossa ovalis. These barriers (lines of
conduction block) can be functional or anatomical, and are necessary to provide adequate path length for the flutter reentry circuit. The tricuspid annulus forms the anterior border of the flutter circuit,
whereas the posterior border occurs at a variable distance from this anterior border; it is narrowest in the region of the eustachian ridge and widest in the anterior part of the RA. Typical AFL is of two types, counterclockwise and clockwise.2 In counterclockwise AFL, activation proceeds caudocephalic up the septal side of the tricuspid annulus toward the crista terminalis and moves cephalocaudal along the lateral wall of the RA to reach the lateral tricuspid annulus, after which it propagates through the isthmus defined by the IVC, CS, and tricuspid annulus (counterclockwise as viewed in the left anterior oblique [LAO] view from the ventricular side of the tricuspid annulus). The circuit is entirely in the RA. In clockwise (reverse typical) AFL, activation propagates
in the opposite direction
ELECTROCARDIOGRAPHIC FEATURES
Typical Atrial Flutter P Waves. Flutter waves appear as atrial complexes of constant morphology, polarity, and CL. Typically, flutter waves are most prominent in the inferior leads (II, III, aVF)
and V1. In the inferior leads, they appear as a picket fence varieties coexist with tall positive, small positive, or biphasic (sawtooth) because the leads are primarily negative. This consists of a downsloping segment, followed by a sharper negative deflection, and then a sharp positive deflection,
with a positive overshoot leading to the next downsloping plateau. The relative size of each component can vary markedly. Counterclockwise AFL can be characterized by pure negative deflections in the inferior leads, negative and then positive deflections that are equal in size, or a small negative and then a larger positive deflection. Those three P waves in V1, respectively. The degree of positivity in the inferior leads appears to be related to the coexistence of heart disease and LA enlargement. Counterclockwise AFL will always have a negative deflection preceding the positive deflection in the inferior leads. Leads I and aVL characteristically show low-voltage deflections. Clockwise AFL generally has broad positive deflections in the inferior leads and wide negative deflections in V1.
Reference
Issa Z, Miller JM, Zipes DP. Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald's Heart Disease: Expert Consult: Online and Print. Elsevier Health Sciences; 2012 Apr 24.