A 50year old male came to JIPMER Pondicherry, India with chief complaints of atypical chest pain on and off since last one week. There was no history of giddiness, syncope, palpitation, family history of sudden cardiac death. There was no past history of diabetes mellitus, hypertension, coronary artery diseases. ECG of the patient is shown below.ECHO heart of the patient was normal.
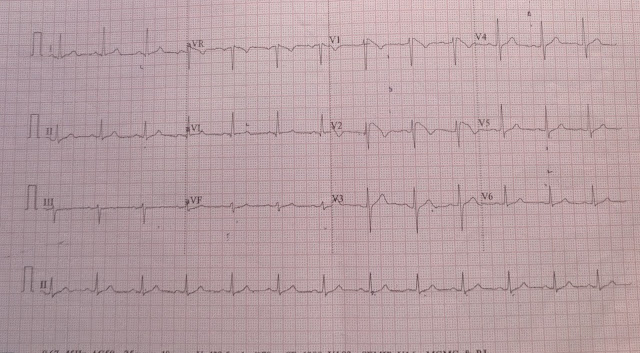
ECG 1


ECG is showing ST elevation in lead V1,V2
ECG of the patient was suggestive of incomplete RBBB with Type I Burgada pattern of ECG.
Cardiac marker of the patient were negative. TMT of the patient , there was no evidence of inducible ischemia.
So on the basis of ECG patient diagnosis is Brugada syndrome (asymptomatic). Because patient was asymptomatic so patient was advised to follow up in cardiology OPD of JIPMER hospital.
Brugada syndrome
Emedicine
Brugada syndrome is a disorder characterized by sudden death associated with one of several ECG patterns characterized by incomplete right bundle-branch block and ST-segment elevations in the anterior precordial leads.
Thank you.
ECG 1
Normal sinus rhythm at 75 beats/min, normal axis, there is rSr pattern seen in lead V1, no other ST-T wave changes seen, PR interval 120 msec, QT interval 360 msec
Patient ECG repeated after 10 minute
ECG 2
ECG is showing ST-segment elevation with T wave inversion in lead V1, V2. ST-segment elevation in lead V1 is 2 mm, in lead V2 is 4 mm
ECG 3
ECG after 20 minute shows ST segment elevation of 3 mm in lead V1 and 5 mm in lead V2
ECG 4

ECG after 30 minute shows ST segment elevation of 3 mm in lead V1 and 5 mm in lead V2
ECG 5

ECG is showing ST elevation in lead V1,V2
ECG 6
ECG is showing ST elevation in lead V1,V2
ECG of the patient was suggestive of incomplete RBBB with Type I Burgada pattern of ECG.
Cardiac marker of the patient were negative. TMT of the patient , there was no evidence of inducible ischemia.
So on the basis of ECG patient diagnosis is Brugada syndrome (asymptomatic). Because patient was asymptomatic so patient was advised to follow up in cardiology OPD of JIPMER hospital.
Brugada syndrome
Emedicine
Brugada syndrome is a disorder characterized by sudden death associated with one of several ECG patterns characterized by incomplete right bundle-branch block and ST-segment elevations in the anterior precordial leads.
Brugada syndrome has three different ECG patterns (Wikipedia)
- Type 1 has a coved type ST elevation with at least 2 mm (0.2 mV) J-point elevation and a gradually descending ST segment followed by a negative T-wave.
- Type 2 has a saddle-back pattern with a least 2 mm J-point elevation and at least 1 mm ST elevation with a positive or biphasic T-wave. Type 2 pattern can occasionally be seen in healthy subjects.
- Type 3 has either a coved (type 1 like) or a saddle-back (type 2 like) pattern, with less than 2 mm J-point elevation and less than 1 mm ST elevation. Type 3 pattern is not rare in healthy subjects.
Signs and symptoms
Signs and symptoms in patients with Brugada syndrome may include the following:
- Syncope and cardiac arrest: Most common clinical manifestations; in many cases, cardiac arrest occurs during sleep or rest
- Nightmares or thrashing at night
- Asymptomatic, but routine ECG shows ST-segment elevation in leads V1-V3
- Associated atrial fibrillation (20%) [1]
- Fever: Often reported to trigger or exacerbate clinical manifestations
The lack of a prodrome has been reported to be more common in patients with ventricular fibrillation documented as the cause of syncope in patients with Brugada syndrome.
Diagnosis
Most patients with Brugada syndrome have a normal physical examination. However, such an examination is necessary to exclude other potential cardiac causes of syncope or cardiac arrest in an otherwise healthy patient (eg, heart murmurs from hypertrophic cardiomyopathy or from a valvular or septal defect).
Testing
In patients with suspected Brugada syndrome, consider the following studies:
- 12-lead ECG in all patients with syncope
- Drug challenge with a sodium channel blocker in patients with syncope without an obvious cause
- Electrophysiologic study to determine the inducibility of arrhythmias for risk
Management
To date, the only treatment that has proven effective in treating ventricular tachycardia and fibrillation and preventing sudden death in patients with Brugada syndrome is implantation of an automatic implantable cardiac defibrillator (ICD)




No comments:
Post a Comment