A 53 year old female resident of Thiruvannamalai, Tamilnadu came to JIPMER hospital emergency with chief complaints of 10-12 episodes of generalised tonic-clonic convulsion along with transient loss of consciousness since one day. Loss of consciousness remain for 5-10 seconds and patient regain consciousness on its own. These episode were associated with frothing from the mouth and urinary incontinence. Patient was a known case of diabetes mellitus and hypertension since last 5 years and was on regular treatment. There was no history of coronary artery diseases, tuberculosis or any other major illness. During evaluation in the emergency department patient pulse rate was 80 per minute, irregular, Blood pressure was 130/80 mmhg, patient was conscious , cooperative and oriented to time, place, person, there was no focal neurological deficit, Cardiovascular system S1S2 were present, respiratory system bilateral normal vesicular sound were present. ECG of the patient done in the emergency department is shown below.
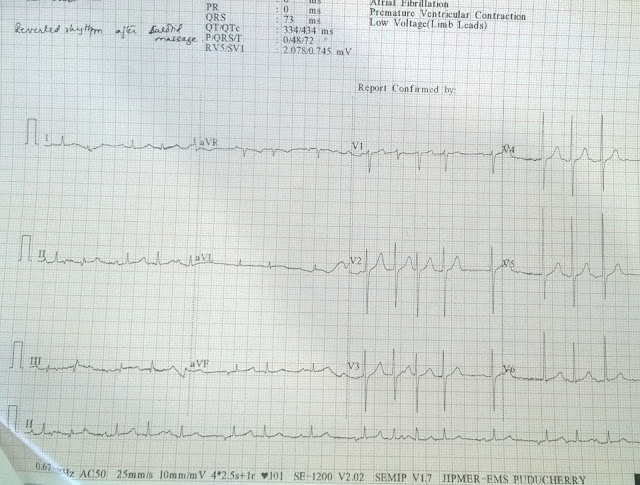
ECG 1(Click on the image to enlarge it )
Description of the ECG-Broad complex tachycardia with QRS of RBBB morphology, QRS duration 140 msec, left axis deviation, P wave are present merged into the QRS complex suggestive of Atrioventricular dissociation, intermittent capture beats are present with normal PR interval, narrow QRS complex, normal axis of sinus beat, so the ecg is suggestive of ventricular tachycardia with RBBB morphology suggestive of origin from the left ventricle.
ECG during sinus rhythm 2
ECG Sinus rhythm at 115 beats per minute, normal axis, PR interval 160 msec, narrow QRS complex, T wave inversion with ST segment flattening present in lead II,III,aVF, V4-V6, Intermittent VPC present with RBBB morphology with left axis deviation with rS in lead V6 present.
So on the basis of above ECG finding patient cardiac marker were sent (Troponin I ) ,which comes within normal limit. Patient echocardiogram done which was suggestive of global hypokinesia of left ventricle with moderate to severe mitral regurgitation, moderate tricuspid regurgitation was present with right ventricular systolic pressure of 40 mmhg. Patient underwent holter monitoring which was suggestive of 60,000 thousands PVC, runs of ventricular tachycardia with RBBB morphology with left axis deviation with rS morphology in lead V6. Patient underwent Coronary angiography which was suggestive of normal coronary.
So the diagnosis of Ventricular tachycardia ??Left posterior fasicular tachycardia ??? Left posterior papillary muscle tachycardia was kept. Patient was planned for electrophysiological study. Patient underwent EPS study which was suggestive of earliest ventricular activation during the VPC close to left ventricle apex close to inferior septum, There was no presystolic purkinje potentials and echocardiogram was suggestive of proximity of this location to the posterior papillary muscle. Pace Mapping from this site showed a 11/12 pace match. Patient underwent successful CARTO guided ablation and later discharged in stable condition.
So the final diagnosis was Idiopathic Left posterior papillary muscle Ventricular tachycardia with tachycardia induced cardiomyopathy.
Little about Idiopathic Left posterior papillary muscle Ventricular tachycardia
VT localized to the base of the Posterior papillary muscle (PPM) in the LV characterized by: (1) a normal baseline ECG and intracardiac conduction intervals with normal LV systolic function; (2) right bundle-branch block and superior-axis QRS morphology; (3) lack of inducibility with programmed ventricular and atrial stimulation; (4) absence of criteria for transient entrainment; (5) inducibility of VT or PVCs with intravenous isoproterenol or epinephrine; (6) earliest ventricular activation at the base of the PPM in the LV; and (7) absence of high-frequency potentials at the site of origin, which suggests that the Purkinje system is not directly involved. Successful catheter ablation at this site uniformly required the use of cooled RF ablation, which suggests that the site of origin was within the papillary muscle itself, somewhat deep within the myocardium.
Reference
Doppalapudi H, Yamada T, McElderry HT, Plumb VJ, Epstein AE, Kay GN. Ventricular Tachycardia Originating From the Posterior Papillary Muscle in the Left VentricleCLINICAL PERSPECTIVE. Circulation: Arrhythmia and Electrophysiology. 2008 Apr 1;1(1):23-9.
Thank you.